Medicine Assignment
Question 1) A 55 year old man with Recurrent Focal Seizures
Detailed patient case report here: http://ushaindurthi.blogspot.com/2020/11/55-year-old-male-with-complaints-of.html
1. What is the problem representation of this patient and what could be the anatomical site of lesion ?
complaints of Unable to move his right upper limb since 9am yesterday recurrent episodes of seizures since 9 15am yesterday few minutes later he developed a sudden onset, tonic clonic seizures involving his right upper limb and lower limb lasting for 2 minutes following which he had another 8 episodes of focal seizures involving his right upper limb and right lower limb with a 2 minutes of gap between each episode. During these episodes he had uprolling of eyes and wasn’t followed by froth discharge from mouth or tongue bite or any involuntary micturation. He was in postictal confusion lasting for 40 minutes. He was immediately taken to a nearby hospital where he was given certain medications ( not documented) , he apparently had two more episodes of GTCS during his hospital stay. After which he was brought to our hospital.
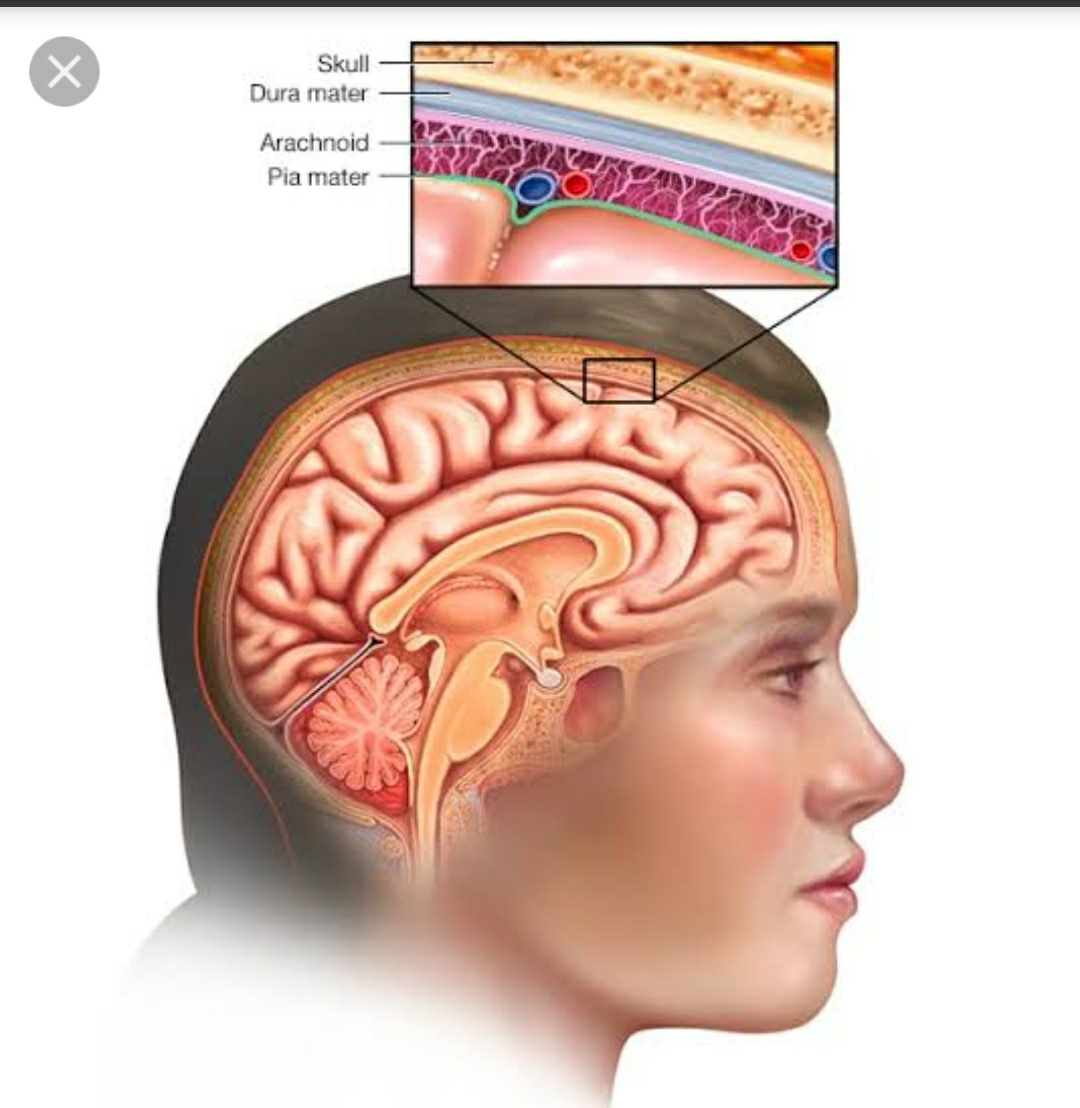
Anatomical site of lesion
Left Frontal lobe infarct
Left Parietal infarct - Primary sensory area (post-central gyrus)
Seizures onset with contralateral (or rarely ipsilateral or bilateral) focal somatosensory seizure
Left Temporal infarct
Left Occipital infarct - Visual hallucinations are the hallmark of occipital seizures, but are not invariably present.
Left Internal capsule infarct - Classic lacunar strokes syndrome that arises from lesions of the internal capsule are pure motor strokes, ataxic hemiparesis, and clumsy hand-dysarthria.
Cerebrovascular accidents are more common in subcortical areas because the perforating arteries that supply the region are predisposed to occlusion or rupture due to their small diameter.
Ischemic strokes secondary to blockage of the perforating arteries are known as lacunar strokes.
The mechanisms of lacunar strokes include
1. Lipohyalinosis of perforating blood vessels - Most common cause
2. Atherosclerosis of the large trunk vessels that supply perforators
3. Embolic occlusion of the perforating arteries.
3. What is the pathogenesis involved in cerebral infarct related seizures?
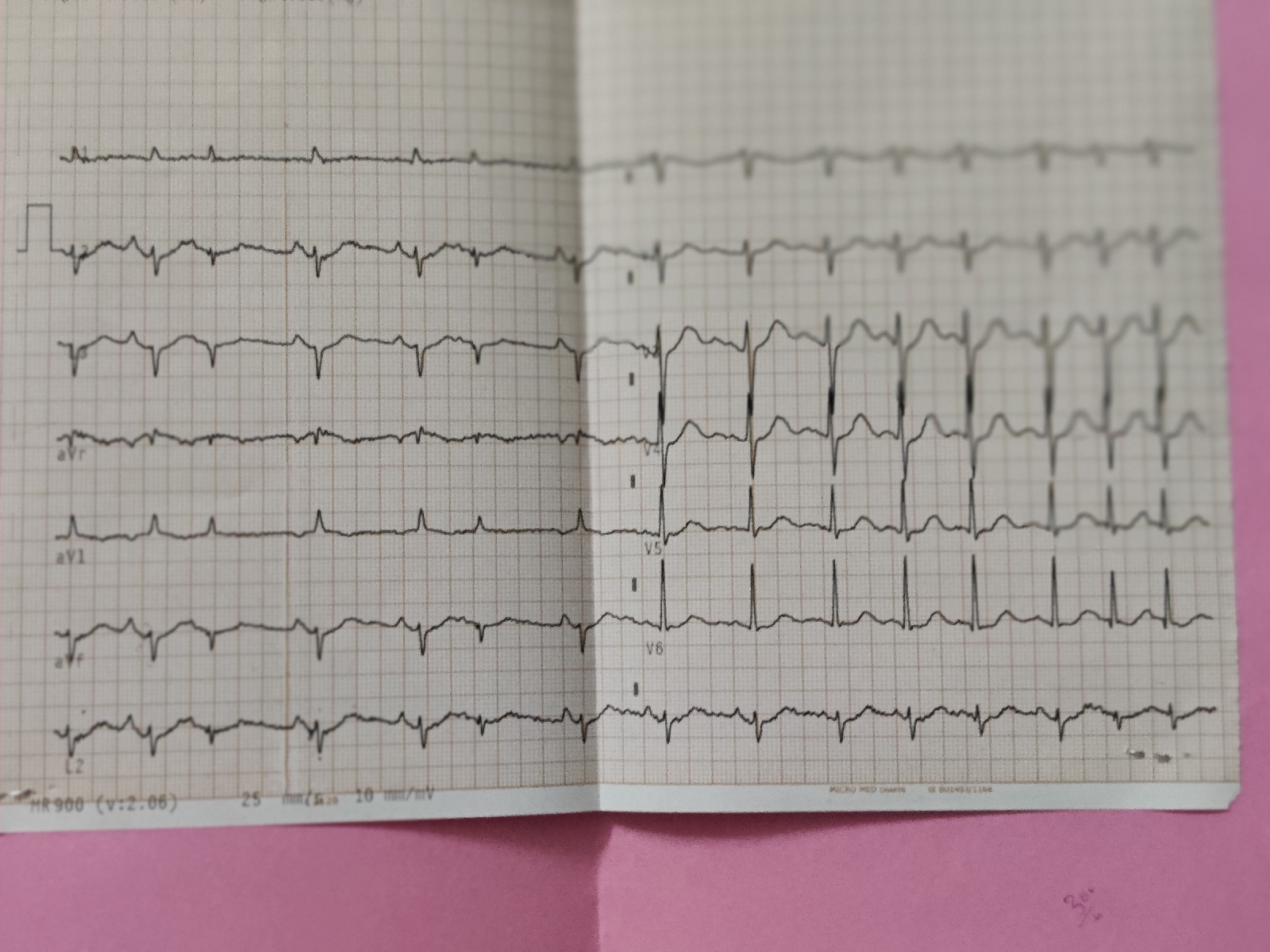
4. What is your take on the ecg? And do you agree with the treating team on starting the patient on Enoxaparin?
ECG shows Sinus Rhythm with LAD, Left Anterior Fasciular Block with VPCS and
NSTEMI in septal leads ( seen on the day of admission -28/11/2020 and in anteroseptal leads on 30/11/2020)
Yes , i agree with the treating team on starting the patient on Enoxaparin.
5. Which AED would you prefer?
As it is focal seizure i would prefer carbamazepine
And lorazepam / diazepam to prevent the conversion of focal seizure to GTCS
Antiepileptics
Atorvastatin
Aspirin
Enoxaparin
If so why?
Please provide studies on efficacies of each of the treatment given to this patient.
Question 2) 55 year old man with Recurrent hypoglycemia
http://manojkumar1008.blogspot.com/2020/12/shortness-of-breath-with-high-sugars.html
Questions:
1. What is the problem representation for this patient?
c/o of Sob ( grade 2-3) which is insidious on onset , progressive , increased on exertion since 3 days c/o cough since 3 days not associated with sputum with grbs - 34mg/dl
2. What is the cause for his recurrent hypoglycemia? And how would you evaluate?
3. What is the cause for his Dyspnea? What is the reason for his albumin loss?
His chest Xray PA shows cardiomegaly with right pulmonary artery prominence with ? Pleural effusion probably secondary to Hypoalbuminemia and right sided consolidatory changes.
As the patient has been complaining of Dyspnea along with non productive dry cough the cause is probably due to Respiratory tract infection but i would also like to have a look at the patients 2Decho.
Albumin loss - Is clearly explained by the renal failure in this patient - with the significant spot pc ratio 3.91 and high serum creatinine 2.7mg/dl.
4. What is the pathogenesis involved in hypoglycemia ?
5. Do you agree with the treating team on starting the patient on antibiotics? And why? Mention the efficacies for the treatment given.
No, i do not agree with the treating team on starting the patient on antibiotics as he has no signs of sepsis
Question 3)
A.41 year old man with Polyarthralgia
Case details here: https://mahathireddybandari.blogspot.com/2020/11/41m-with-chest-pain-and-joint-pains.html?m=1
1. How would you evaluate further this patient with Polyarthralgia?
2. What is the pathogenesis involved in RA?
3. What are the treatment regimens for a patient with RA and their efficacies?
B.
75 year old woman with post operative hepatitis following blood transfusion
Case details here: https://bandaru17jyothsna.blogspot.com/2020/11/this-is-online-e-log-book-to-discuss.html
1.What are your differentials for this patient and how would you evaluate?
Post transfusion delayed hemolytic reaction
Evaluation:
ABO and Rh compatability
coombs testing
antibody panel testing
-Transfusion related acute hepatic injury (TRAHI)
-Post transfusion hepatitis
-Ischemic hepatitis
Evaluation:
2. What would be your treatment approach? Do you agree with the treatment provided by the treating team and why? What are their efficacies?
Symptomatic management
I agree with the treatment provided by the treating team
Lasix & Nebulization : For wheezing and crepts
Lactulose : To prevent hepatic encephalopathy https://pubmed.ncbi.nlm.nih.gov/27089005/
Zofer : For vomitings
Pantop : To prevent gastritis
Question 4) 60 year woman with Uncontrolled sugars
http://manojkumar1008.blogspot.com/2020/12/60-yr-old-female-with-uncontrolled.html
1. What is the problem representation of this patient?
with complaints of chest pain since 4 days pricking type radiating to back relived on medication, no aggravating and relieving factorsGRBS at time of presenting is 585
Burning type of epigastric pain since 3 days
Complaints of constipation since 3 days
Known case of hypertension since 2 yrs ( unknown medication)
DM 2 since 2 years ( unknown medication)
1½ year back patient has fever for 3 days with altered sensorium for 1 day and shortness of breath for 1 day.
Diagnosed as acute kidney injury with septic shock with dyselectrolytemia
History of 1 episode of seizures
2. What are the factors contributing to her uncontrolled blood sugars?
3. What are the chest xray findings?
Hyperdense area noted in the right upper lobe
4. What do you think is the cause for her hypoalbuminaemia? How would you approach it?
Inflammation (acute phase reactant)
Malnutrition
Albuminuria (protein losing nephropathy
5. Comment on the treatment given along with each of their efficacies with supportive evidence.
Piptaz & clarithromycin : for his right upper lobe pneumonic consolidation and sepsis
Egg white & protien powder : for hypoalbuminemia
Lactulose : for constipation
Actrapid / Mixtard : for hyperglycemia
Tramadol : for pain management
Pantop : to prevent gastritis
Zofer : to prevent vomitings
Question 5) 56 year old man with Decompensated liver disease
Case details here:
https://appalaaishwaryareddy.blogspot.com/2020/11/56year-old-male-with-decompensated.html
1. What is the anatomical and pathological localization of the problem?
Liver : Chronic liver disease (cirrhosis) secondary to HBV
Kidney : AKI on CKD (Hepatorenal syndrome) , Hyperkalemia
GI : GAVE , portal hypertensive gastropathy
Lung : pneumonia , pleural effusion
2. How do you approach and evaluate this patient with Hepatitis B?
3. What is the pathogenesis of the illness due to
B?4. Is it necessary to have a separate haemodialysis set up for hepatits B patients and why?
Yes , separate machines must be used for patients known to be infected with HBV (or at high risk of new HBV infection). A machine that has been used for patients infected with HBV can be used again for non-infected patients only after it has been decontaminated using a regime deemed effective against HBV because of increased risk of transmission due to contamination.
https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-019-1529-1
5. What are the efficacies of each treatment given to this patient? Describe the efficacies with supportive RCT evidence.
- Lactulose : for prevention and treatment of hepatic encephalopathy. https://pubmed.ncbi.nlm.nih.gov/27089005/
- Tenofovir : for HBV
- Lasix : for fluid overload (AKI on CKD) https://www.ncbi.nlm.nih.gov/books/NBK499921/#:~:text=The%20Food%20and%20Drug%20Administration,failure%20including%20the%20nephrotic%20syndrome.
- Vitamin -k : for ? Deranged coagulation profile (PT , INR & APTT reports not available)
- Pantop : for gastritis
- Zofer : to prevent vomitings
- Monocef (ceftriaxone) : for AKI (? renal
Question 6) 58 year old man with Dementia
Case details: http://jabeenahmed300.blogspot.com/2020/12/this-is-online-e-log-book-to-discuss.html
1. What is the problem representation of this patient?
2. How would you evaluate further this patient with Dementia?
3. Do you think his dementia could be explained by chronic infarcts?
4. What is the likely pathogenesis of this patient's dementia?
5. Are you aware of pharmacological and non pharmacological interventions to treat such a patient and what are their known efficacies based on RCT evidence?
This international, multicenter, 24-week trial was conducted from March 2003 to August 2005.
P - 974 Patients with probable or possible VaD were randomized 2:1 to receive donepezil 5 mg/d or placebo
I - Donepezil 5mg/d
C - Placebo
O - Patients with hippocampal atrophy who were treated with donepezil demonstrated stable cognition versus a decline in the placebo-treated group; in those without atrophy, cognition improved with donepezil versus relative stability with placebo.
Patients treated with donepezil 5 mg/d demonstrated significant improvement in cognitive, but not global, function. https://pubmed.ncbi.nlm.nih.gov/20395618/
Question 7) 22 year old man with seizures
Case report here http://geethagugloth.blogspot.com/2020/12/a-22-year-old-with-seizures.html
1. What is the problem representation of this patient ? What is the anatomic and pathologic localization in view of the clinical and radiological findings?
22 year old man with complaints of headache since 2 months and involuntary stiffness of bilateral upper and lower limbs since 1 week along with Loss of consciousness.
Anatomical localisation - Brain
Involving both the upper limbs and lower limbs
Could be due to multiple infarcts
Ring enhancing lesions as he is RVD positive
Radiologically
Shows ring enhancing lesions
2. What the your differentials to his ring enhancing lesions?
3. What is "immune reconstitution inflammatory syndrome IRIS and how was this patient's treatment modified to avoid the possibility of his developing it?
A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy in HIV-infected patients is defined as immune reconstitution inflammatory syndrome.
Despite numerous descriptions of the manifestations of IRIS, its pathogenesis remains largely speculative. Current theories concerning the pathogenesis of the syndrome involve a combination of
1. Antigenic burden
2. degree of immune restoration following
3. Host genetic susceptibility
Question 8) Please mention your individual learning experiences from this month.
1.In a case of Hypertensive emergency, giving nicardia for response atleast 2-3 times every 20 min if the Bp still same then admistering Nitroglycerin infusion after sometime on regular monitoring if there is decrease in Bp then tappering dose of NTG according to patients response.
2.Foacal seizures management with levipil and carbamazepine
3.Acute pancreatitis case management
4.ECG interpretation
5.LFT interpretation and ruling out the differential causes
6.RFT interpretation
7.ABG interpretation and sample taking method.
8.Postural BP monitoring.




Comments
Post a Comment