Medicine assessment January
"This is my submission for the Bimonthly internal assessment for the month of January."
Most of the information here have been collected from different reference sites, links to which have been mentioned.The points copy pasted have been put in quotes.
The questions to the cases being discussed are from the link below:
26 year old woman with complaints of altered sensorium somce 1 day,headache since 8 days,fever and vomitings since 4 days
a) what is the problem representation of this patient and what is the anatomical localisation for her current problem based on her clinical findings.
Answer) This is a case of 26 year female who had history of headaches since 1 month which was relieved on taking medication
Since the last 8 days she has bitemporal vertex headache since 8 days after she stopped using SLE medication
following that she had headache,neckpain and fever
She was admitted in a local hospital and at night of admission ,she was noticed lying on the floor of bathroom in altered sensorium
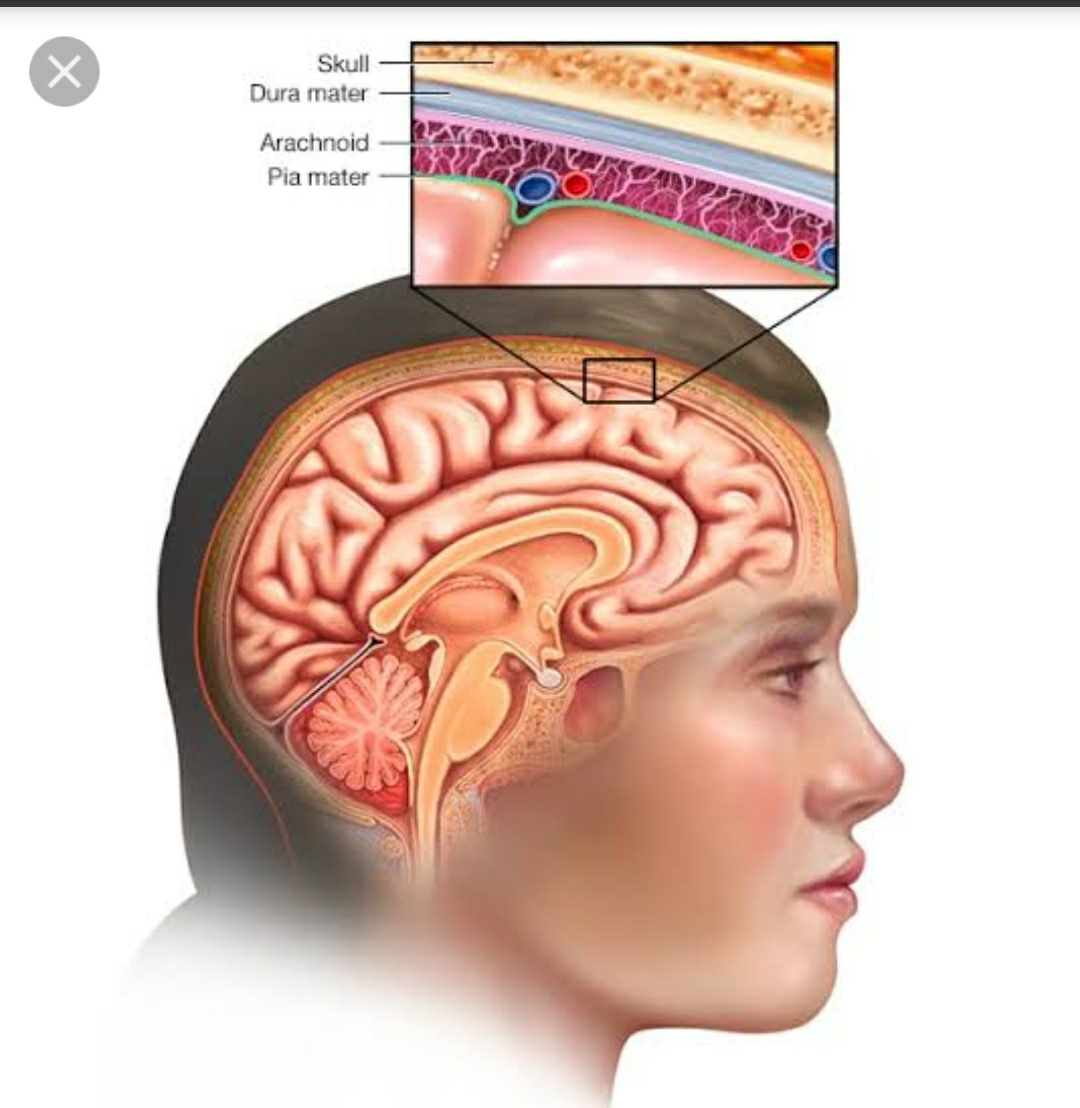
Anatomical localisation- she has chronic headache and neck pain along with altered sensorium-the reason might be meningitis which has gone in to encephalopathy
Differentials are she is also a patient of SLE who stopped medication 10 days ago it might be a case of SLE encephalitis
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of her problems and current outcomes.
According to The patient history,the etiology is mycobacterium tuberculosis,also the CBNAAT done for csf is positive,indicating tubercular meningitis,the source of infection is father in law who tested positive for CBNAAT and completed ATT therapy
To arrive at a diagnosis,for chronic headache CT or MRI is the preferred modality,MRI was done and it revealed focal acute infarcts in the left thalamus.
And as to why the patient is in delirium the causes might be
Also lumbar puncture was done it revealed normal protein and cell count but the glucose levels were decreased.
In meningitis generally the glucose levels in CSF are decreased as they are utilised by bacteria and cell count is raised and proteins are also elevated
Sequence of events:
Patient had bilateral hands small joint pains, 6 years back which later involved her shoulders and elbows for which she took medication prescribed by a local medical shop for about 10 days and stopped using the medicine after that duration.
Later 3 years back, she developed multiple joint pains for which she visited local hospitals and then got diagnosed with SLE in NRI hospitals and is using SLE medication including
Hydroxychloroquine,sulfasalazine,methylprednisolone,aceclofenac,cholecalciferol,alandronic acid, flupirtine ,gabapentin ,methylcobalamine tablets.
The patient had low grade fever and joint pains whenever she would miss her SLE medication.
Since 1 month she has episodes of headache 1-2 times per week,she stopped using SLE medication 15 days after that,and following which she developed fever and neck pain and the headache has become continuous after few days
Later the patient was unable to walk,has generalised weakness, decreased appetite for which she was admitted in Nalgonda and at night of admission she went to washroom and then felt unconscious,she was brought to casualty with an altered sensorium and irrelavent talk
c) What is the efficacy of each of the drugs listed in her prior treatment plan that she was following since last two years before she stopped it two weeks back?
Hydroxychloroquine,
sulfasalazine,
methylprednisolone,
aceclofenac
cholecalciferol,
alandronic acid,
flupirtine ,
gabapentin ,
methylcobalamine tablets.
Hydroxychloroquine in SLE
“Chloroquine, together with its hydroxyl derivative hydroxychloroquine, was initially used as an antimalarial agent, but is also useful in the treatment of autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus (SLE).
Chloroquine and hydroxychloroquine are approved for the treatment of SLE and have been shown to reduce the frequency of disease flares (particularly of lupus nephritis), contribute to the maintenance of remission, prolong the onset of disease and reduce the risk of complications.Beyond their immunomodulatory effects in SLE, these agents have also been shown to protect against thrombotic events, improve glucose and lipid profiles, and prevent renal damage,apparently resulting in reduced cardiovascular risk, for which SLE is an independent risk factor”
Sulfasalazine:
Immunosuppressive drug used in the treatment of cutaneous manifestations of lupus.
“Sulfasalazine is an effective agent for chronic discoid lupus erythematosus (CDLE) but the response to treatment is considerably variable between patients and is also unpredictable. The reason for this might relate to differences in metabolism of the drug which is extensively acetylated by the polymorphic enzyme N-acetyltransferase 2 (NAT2). To test this possibility, the N-acetylation phenotype of eleven patients with CDLE and treated by standard doses of sulfasalazine was retrospectively determined by genotyping. A clear-cut difference in the outcome of treatment was observed according to whether the patients were slow acetylators (SA) or rapid acetylators (RA). Eight out of 11 patients responded to treatment with a complete or marked remission of the disease. Seven of them were RA. The three other patients who did not respond at all to the drug were SA. In addition, SA seem to be more prone to toxic events. These findings strongly suggest that the genetic polymorphism of NAT2 is responsible for differences in the response to sulfasalazine in patients with CDLE. Therefore, candidates for sulfasalazine therapy should be genotyped to identify those patients who might benefit from the drug.”
Methyl prednisolone: Glucocorticoids (GCs) are the mainstay of treatment of SLE as induction therapy and to manage acute flares and have dramatically improved the prognosis of severe SLE.
Intravenous (IV) pulse methylprednisolone therapy, mostly 500-1,000 mg daily for 1-3 days, was introduced in the 1970s (Cathcart, 1976) and is remarkably efficacious in critically ill patients (Isenberg, 1982), suffering renal impairment, central nervous system disease, severe arthritis, pleuropericarditis or thrombopenia.There is still a doubt regarding tapering of the dose of IV methylprednisolone needed to achieve rapid control of activity .
Tapering schedules are mainly based on physician’s experience and clinical judgment.
In patients requiring the therapy adequate prevention of bone loss should be applied, keeping in mind that GC-induced osteoporosis is an early event. Patients must be immunized against influenza (every year) and Streptococcus pneumoniae (every 5 years)
Aceclofenac:
“The therapeutic effect of NSAIDs is determined by the suppressed activity of the cyclooxygenase (COX) isoenzymes COX- 1 and COX-2. The widely use of NSAIDs in clinical practice is considerably limited by the risk of adverse reactions (ARs) in the gastrointestinal tract (GIT), which are characteristic for this class of drugs. Medications that are able to selectively inhibit the activity of COX-2 while maintaining that of COX-1 less rarely cause ARs in GIT. This selective effect is produced by aceclofenac. The drug has been also noted to be well tolerated: the risk for aceclofenac- induced ARs in GIT is substantially lower than that due to the use of the majority of other NSAIDs”.
Source:
cholecalciferol
There is a protective effect of Vitamin D on the immunological abnormalities associated with SLE including its association with downregulation of the T-cell response, proliferation of B-cells, and upregulation of Tregs.
Alandronic acid:
for the prevention and treatment of osteoporosis in Glucocorticoid ‐treated individuals without renal impairment
Flupirtin: used as an analgesic for chronic and acute pain
Gabapentin
Methyl cobalamin
d) Please share any reports around similar patients with SLE and TB meningitis?
Tubercular meningitis (TBM) is a rare condition in patients with systemic lupus erythematosus (SLE). The aim of this study is to describe the clinical characteristics, possible risk factors, and outcomes of SLE patients with TBM.
On systematically reviewing medical records from10 SLE patients with TBM admitted to a hospital from December 2008 to December 2018. A total of 100 cases in the same period were randomly selected as controls from SLE inpatients without infection. In patients with TBM, the mean age at presentation was 35.2 years (range 19.8–45.2); the mean duration of SLE was 34.6 months (range 4–84 months). Patients with TBM had significantly longer SLE duration, higher ESR and CRP level, and lower CD4+ cell counts and albumin level than those without infections (p < 0.05 for all). There were no differences in prednisone dose at the time of symptom onset or cumulative dose over the preceding year between the two groups. Logistic regression analysis showed that patients with a lower CD4+ cell count were more likely to have TBM compared with controls (OR = 3.67, p = 0.020).
TBM should be considered when SLE patients have central nervous system (CNS) symptoms with a longer duration, higher ESR and CRP level, and lower CD4+ cell counts and albumin level, even if the patients are receiving a low prednisone dose,and the patient being studied has a chronic headache and fits into this criteria
Any reports of normal csf leukocyte count and normal csf protein in meningitis?
What could be the probable cause for a normal csf leukocyte count in a patient with chronic meningitis?
e) What is the sensitivity and specificity of ANA in the diagnosis of SLE?
Methods: Retrospective chart review in a 400-bed teaching hospital in which 1010 patients (including inpatients and outpatients) for whom ANA testing was ordered over 10 months; all patients with positive ANA test results and an equal number of randomly selected patients with negative test results were included. Clinical utility of the ANA in the identification of rheumatic disease was determined by its estimated sensitivity, specificity, and positive and negative predictive values.
Results: Of 1010 ANA test results reviewed, 153 were positive. The group with positive ANA test results included more patients aged 65 years or older than the group with negative ANA test results (30% vs 15%, P < .003). The diagnosis of systemic lupus erythematosus (SLE) was established in 17 patients, all of whom had positive ANA test results. Other rheumatic diseases were found in an additional 22 patients. The estimated sensitivity and specificity of the ANA test for SLE were 100% and 86%, respectively. For other rheumatic diseases, sensitivity and specificity were 42% and 85%, respectively. The positive predictive value of the ANA test was 11% for SLE and 11% for other rheumatic diseases. Specificity and positive predictive value for ANA testing in the elderly patients were lower than among younger patients
Conclusions: sensitivity of the ANA test for SLE was high, but overall the positive predictive value was low for SLE or other rheumatic diseases. Sensitivity was low for ANA testing among patients with non-SLE rheumatic disease. More selective test ordering might improve the clinical utility of this test. Clinicians ordering the ANA test should be aware of the test's low-positive predictive value in settings with a low prevalence of rheumatic disease, particularly among older patients.
2) Please go through the two thesis presentations below and answer the questions below by also discussing them with the presenters:
1)What was the research question in the above thesis presentation?
To study the association of serum magnesium levels of type 2 diabetes mellitus
2) What was the researcher's hypothesis?
Normal magnesium levels are 1.6 to 2.4
Where as in diabetics substantial amount of population have a low magnesium levels in the blood, also in non diabetic populations, a low magnesium level is a danger sign that the person might develop diabetes mellitus
Magnesium deficiency is associated with hypocalcemia, hypokalemia and arrhythmias and hence correlates with a higher mortality /morbidity
If There is reduced serum magnesium they have a negative impact on glucose homeostasis and insulin sensitivity,leading to early development of complications such as nephropathy,neuropathy and retinopathy and thus have worst outcomes compared to people who are diabetic and have normal magnesium levels.
The diabetic complications progress faster in these populations
3) What is the current available evidence for magnesium deficiency leading to poorer outcomes in patients with diabetes?
“Hypomagnesemia occurs at an incidence of 13.5 to 47.7% among patients with type 2 diabetes. Poor dietary intake, autonomic dysfunction, altered insulin metabolism, glomerular hyperfiltration, osmotic diuresis, recurrent metabolic acidosis, hypophosphatemia, and hypokalemia may be contributory. Hypomagnesemia has been linked to poor glycemic control, coronary artery diseases, hypertension, diabetic retinopathy, nephropathy, neuropathy, and foot ulcerations. The increased incidence of hypomagnesemia among patients with type 2 diabetes presumably is multifactorial. Because current data suggest adverse outcomes in association with hypomagnesemia, it is prudent to monitor magnesium routinely in this patient population and treat the condition whenever possible.”
In addition to hyperosmolar coma and ketoacidosis, patients with type 2 diabetes may have cardiovascular disease, nephropathy, retinopathy, and polyneuropathy. With its associated complications, diabetes was reported to be the sixth leading cause of death. numerous studies have reported an inverse relationship between glycemic control and serum Mg levels. In patients with type 2 diabetes, oral Mg supplementation during a 16-wk period was suggested to improve insulin sensitivity and metabolic control
There is a correlation between glycemic control and serum Mg levels or improvement of diabetic control with Mg replacement
Cardiovascular.
In a study that involved 19 normotensive individuals without diabetes, 17 hypertensive individuals without diabetes, and 6 hypertensive individuals with diabetes, Resnick et al. documented the lowest mean intracellular Mg concentration among the last group. Similarly, based on data from the Atherosclerosis Risk in Communities (ARIC) Study, a multicenter, prospective cohort study that lasted 4 to 7 yr and involved 13,922 middle-aged adults who were free of coronary heart disease at baseline, an inverse association between serum Mg and the risk for coronary heart disease was observed among men with diabetes
Diabetic Retinopathy.
The link between hypomagnesemia and diabetic retinopathy was reported in two cross-sectional studies that involved both “insulin-dependent” patients and patients with type 2 diabetes. Not only did patients with diabetes have lower serum Mg levels compared with their counterparts without diabetes, but also the serum Mg levels among the cohort with diabetes had an inverse correlation with the degree of retinopathy .
Foot Ulcerations.
Given the link between hypomagnesemia and risk factors for the development of diabetic foot ulcers (e.g., polyneuropathy, platelet dysfunction), Rodriguez-Moran and Guerrero-Romero (48) suggested that hypomagnesemia may be associated with an increased risk of diabetic foot ulcers. Indeed, they observed a higher incidence of hypomagnesemia among their patients with diabetic foot ulcers compared with those without the condition (93.9% of the 33 patients with diabetic foot ulcers compared with 73.1% of the 66 patients without diabetic foot ulcers; P = 0.02).
Nephropathy.
In a comparative study that involved 30 patients who had type 2 diabetes without microalbuminuria, 30 with microalbuminuria, and 30 with overt proteinuria, Corsonello et al. (49) observed a significant decrease in serum ionized Mg in both the microalbuminuria and overt proteinuria groups compared with the nonmicroalbuminuric group. Accordingly, in a recent retrospective study, an association between low serum Mg levels and a significantly faster rate of renal function deterioration in patients with type 2 diabetes was reported (7).
Others.
Finally, there also are data to suggest the association between hypomagnesemia and other diabetic complications, including dyslipidemia and neurologic abnormalities.Because hypomagnesemia has been linked to various micro- and macrovascular complications, a better understanding of Mg metabolism and efforts to minimize hypomagnesemia in the routine management of diabetes are warranted.
Source:
Magnesium Deficiency and Type 2 DiabetesMagnesium plays an important role in carbohydrate metabolism. It may influence therelease and activity of the hormones that helps control blood glucose levels [56]. Low bloodlevels of magnesium are frequently observed in individuals with type 2 diabetes [57].Hypomagnesemia may worsen insulin resistance, a condition that often precedes diabetes,or may be a consequence of insulin resistance. Individuals with insulin resistance cannotuse insulin efficiently and require greater amounts of insulin to maintain blood glucosewithin normal levels. Kidneys possibly lose their ability to retain magnesium during periodsof severe hyperglycemia. The increased loss of magnesium in urine may then result inlower blood levels of magnesium in older adults, and correcting magnesium depletion mayimprove insulin response and action
Magnesium Deficiency and Type 2 DiabetesMagnesium plays an important role in carbohydrate metabolism. It may influence therelease and activity of the hormones that helps control blood glucose levels [56]. Low bloodlevels of magnesium are frequently observed in individuals with type 2 diabetes [57].Hypomagnesemia may worsen insulin resistance, a condition that often precedes diabetes,or may be a consequence of insulin resistance. Individuals with insulin resistance cannotuse insulin efficiently and require greater amounts of insulin to maintain blood glucosewithin normal levels. Kidneys possibly lose their ability to retain magnesium during periodsof severe hyperglycemia. The increased loss of magnesium in urine may then result inlower blood levels of magnesium in older adults, and correcting magnesium depletion mayimprove insulin response and action
What was the research question in the above thesis presentation?
To study the 24 hour urinary sodium secretion in newly diagnosed hypertensive patients
Objectives: to analyse the 24 hour urinary sodium with respect to stages of hypertension
To study effects of sodium on BMI
analyse 24 hour urinary sodium excretion in complications of hypertension which include opthalmic,renal and cardiovascular changes.
What was the researcher's hypothesis?
Researcher wanted to find out whether salt restriction in hypertensive patients,as hgave some sort of benefit to them,but in reality there are two categories of patients salt sensitive
and insensitive groups.It is estimated that 50-60% are salt sensitive and only the sensitive group reacts to changes in dietary salt intake with alterations in blood pressure. It is estimated that about 50-60 % of hypertensives are salt sensitive
To find out this 24 hour urinary sodium excretion was assessed in
Tot
What is the current available evidence for the utility of monitoring salt excretion in the hypertensive population?
High dietary intake of sodium is seen in most of the subjects who have very high blood pressures
By the means of a self monitoring device
Subjects were 34 hypertensive patients who underwent successful 24-h home urine collection five times and 25 volunteers. Four volunteers were diagnosed as having hypertension based on home blood pressure (BP) readings. All subjects were asked to measure daily urinary salt excretion for 30 days by using a self-monitoring device which estimates 24-h salt excretion by overnight urine. The mean urinary salt excretion during the 30 days was 8.36 +/- 1.52 g/day and the range (maximum-minimum value) was 5.47 +/- 20.05 g/day in all subjects. Mean urinary salt excretion decreased from 8.52 +/- 1.63 g/day for the first 10 days to 8.31 +/- 1.54 g/day for the last 10 days (p < 0.05). The mean urinary salt excretion determined by a self-monitoring device using overnight urine was positively associated with that determined by 24-h home urine for five times in the hypertensive subjects (r = 0.63, p < 0.01). Results indicate that a self-monitoring device seems to be useful to monitor daily salt intake and to guide salt restriction.
This might be useful in subjects who are sensitive to sodium restriction
Source:
3)Please critically appraise the full text article linked below:
What is the efficacy of aspirin in stroke in your assessment of the evidence provided in the article. Please go through the RCT CASP checklist here https://casp-uk.net/casp-tools-checklists/ and answer the questions mentioned in the checklist in relation to your article.
Clinical appraisal of the article:
1)The study answered the research question
being the use of asprin for prevention of stroke progression.
it was foccused in terms of intervention given and outcome measured
2)the method for randomisation was appropriate eliminating systematic bias and allocation sequence concealed from investigators and participants
3)all the participants included in the study were accounted for, including rhe two parcels whixh were accidentally opened.
4)the participants and the investigators were blind methodically
5)the study groups were similar
6)apart from the experimentation, the hospital care given is not documented
7)there were dropouts in the study, study medication was interrupted in few due to suspected side effects,
the p value was not mentioned
8)the cI interval 95%0.6-1.45
9)the treatment effect wasn't much,
10)the outcomes are benefial to my population in prescribing anticoagulants
dual vs single antiplatelet use and longer duration of followup could have been made .
4) Please mention your individual learning experiences from this month.
Learned how to do 2d echo and its interpretation
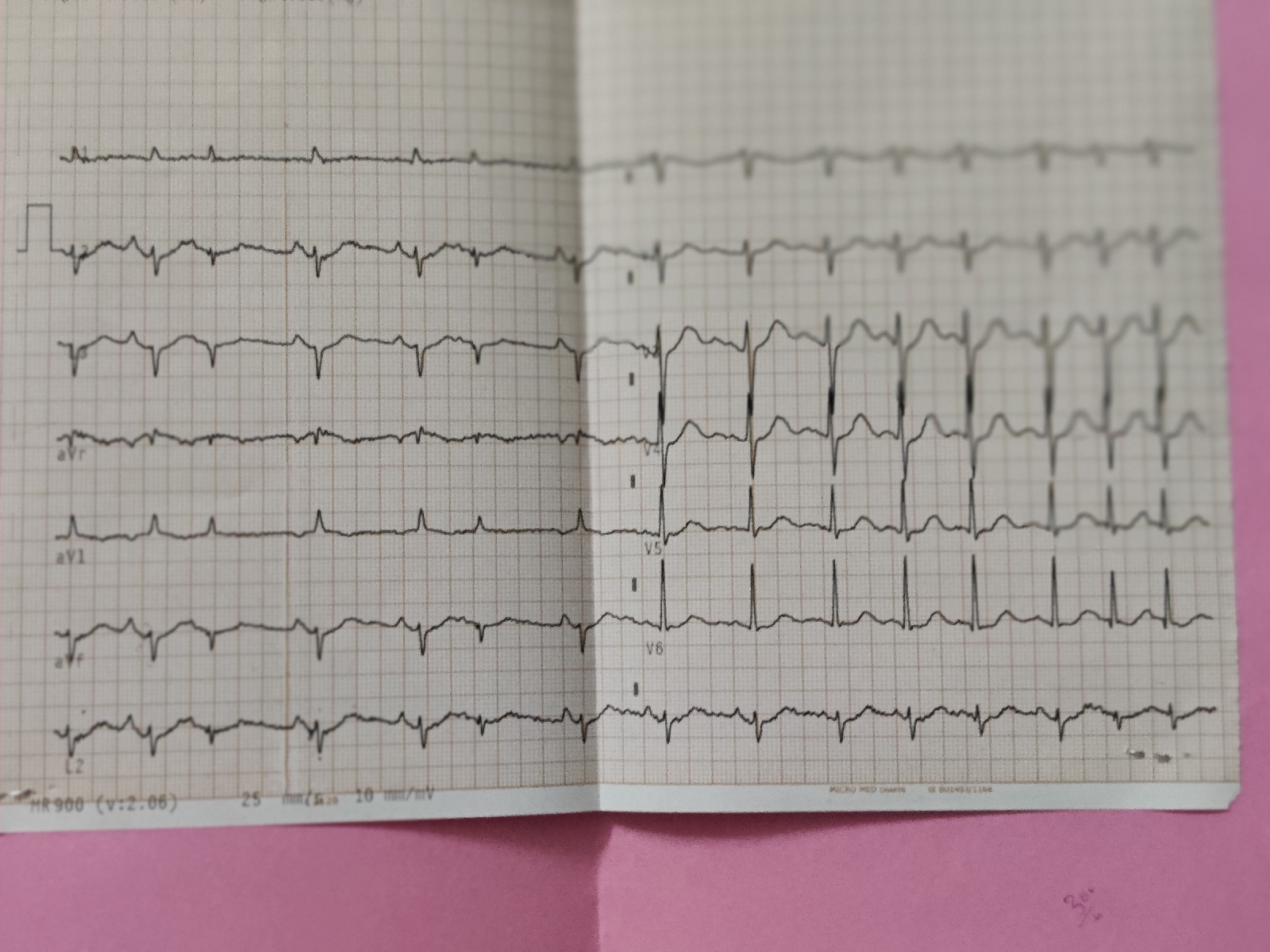
Interpretation of ECG
Interpretation of hemogram
Procedure of how to put a central line (CVP)
Different drugs used in SLE and their efficacies and SLE association with meningitis
How to do the procedure of pleural tap
Procedure to remove excess pericardial fluid
5) a) What are the possible reasons for the 36 year old man's hypertension and CAD described in the link below since three years?
The possible reasons for hypertension and cad in the given history could be
Alcohol
The HPFS is a prospective investigation of 51 529 US male dentists, pharmacists, veterinarians, optometrists, osteopathic physicians, and podiatrists aged 40 to 75 years who returned a mailed questionnaire about diet and medical history in 1986.
At baseline, men reported their alcohol consumption on a 131-item semiquantitative food frequency questionnaire (FFQ) that included separate items for beer, white wine, red wine, and liquor. Participants were asked how often, on average over the past year, they consumed each beverage. We calculated total alcohol intake by multiplying the average consumption of each beverage by the alcohol content of the specified portion size (12.8 g for beer, 11.0 g for wine, and 14.0 g for liquor) and summing across beverages. The FFQ was administered again every 4 years, with an item for light beer added in 1994. Participants also reported their overall drinking frequency in 1986, 1988, and 1998.
results:
When we compared alcohol intake of 5.0 g/d or more vs less than 5.0 g/d, the hazard ratio was 0.58 (95% CI, 0.37-0.89). Given that 55% of person-time was contributed by consumers of 5 g/d or more of alcohol, we estimate that 25% of the incidence cases of MI in this population were attributable to consuming less than 5 g/d (95% CI, 11%-47%).
Smoking
Temporal Associations Between Smoking and Cardiovascular Disease, 1971 to 2006 (from the Framingham Heart Study)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6541867/
b) Please describe the ECG changes and correlate them with the patient's current diagnosis.
The ecg suggests:
1st ecg-irregularly irregular rythmn,normal axis,
Intermittent broad qrs complexes ? ventricular escape rythmn,?idioventricular rythmn
Remaining ecg-poor r wave progression with regular rythmn
c) Share an RCT that provides evidence for the efficacy of primary PTCA in acute myocardial infarction over medical management. Describe the efficacy in a PICO format.
RITA-2 is a randomized control trial published in
Journal of the American College of Cardiology Clinical Trials Vol. 42, No. 7, 2003 © 2003 by the American College of Cardiology Foundation Published by Elsevier Inc.
P-1018,Patients were recruited at 20 centers in the U.K. and Ireland. In brief, patients with arteriographically proven coronary artery disease (CAD) were considered for the trial if the supervising cardiologist thought that continued medical therapy and PTCA were both acceptable treatment options. Patients had to be over 18 years of age, but there was no upper age limit.
I-The 1,018 patients were randomized to coronary angioplasty (n 504) or continued medical treatment (n 514) from July 1992 to May 1996. Follow-up to September 30, 2001, is included in this report, the median follow-up period being seven years.
C-compared based on death and MI
subsequent interventions required
relief of symptoms of angina and breathlessness
O-Death or myocardial infarction (MI) occurred in 73 (14.5%) PTCA patients and 63 (12.3%) medical patients (difference 2.2%, 95% confidence interval 2.0% to 6.4%, p 0.21). There were 43 deaths in both groups, of which 41% were cardiac-related. Among patients assigned PTCA 12.7% subsequently had coronary artery bypass grafts, and 14.5% required additional non-randomized PTCA. Most of these re-interventions occurred within a year of randomization, and after two years the re-intervention rate was 2.3% per annum. In the medical group, 35.4% required myocardial revascularization: 15.0% in the first year and an annual rate of 3.6% after two years. An initial policy of PTCA was associated with improved anginal symptoms and exercise times. These treatment differences narrowed over time, mainly because of coronary interventions in medical patients with severe symptoms



Comments
Post a Comment